It’s a fact of life that as we age, our bodies grow older right along with us. Our vision starts to blur, our joints start to ache and according to experts, our blood pressure almost certainly will begin to rise. As the baby boomers approach retirement and Gen Xers reach middle age, the number of older Americans is increasing at a frenzied pace as we live longer, but not necessarily healthier, lives.
According to an article published by the American College of Cardiology, geriatric cardiologists should start preparing to care for patients in their 80s, 90s and beyond, as life expectancy continues to rise. With hypertension occurring in up to 80 percent of people over the age of 60, physicians have their work cut out for them in caring for this aging population.
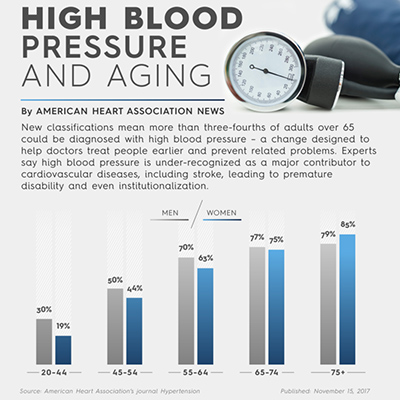
Due to the American Heart Association’s (AHA) recently released new guidelines for categorizing blood pressure, nearly half of all American adults are considered to have hypertension, but not all health organizations agree on how to best care for older adults with high blood pressure. The AHA’s new standards mean that older adults between the ages of 65 and 74 will be newly categorized as hypertensive at an increased rate of 13 percent for men and 12 percent for women.
Arash Tirandaz, M.D., internist and physician on the medical staff at Texas Health Plano, says regardless of the AHA’s new guidelines, physicians must approach each patient individually to evaluate his or her overall health and risk factors before deciding on a course of treatment.
“Nothing is one-size-fits-all, but in general the risk of heart attack and stroke goes up as we get older, so we need to be more careful that the blood pressure is not too high or too low,” he explains. “Preventing heart attacks and stroke is what it’s all about.”
Last March, the American College of Physicians (ACP) and American Academy of Family Physicians (AAFP) recommended that physicians wait to treat patients over the age of 60 for high blood pressure until their systolic level was persistently at or over 150 mm Hg. For patients with a history of stroke or those with high cardiovascular risk, the recommended threshold for treatment was lowered to 140 mm Hg.
Authors of the article recognize the physical and financial impact ($45+ billion annually) of hypertension among older Americans, and say finding the right balance between lifestyle changes and pharmacological interventions is important due to potential side effects and impacts on comorbid conditions. They also say physicians should take into consideration a patient’s medication burden, risk for adverse reactions and cost when considering treatment for hypertension.
In response, the AHA released a statement from their president, Steven Houser, Ph.D., voicing his concern over a less aggressive approach to treating hypertension in older adults. Houser points to the reduction of blood pressure as imperative in reducing the risk for heart failure and stroke, and adds that raising the threshold of treatment could potentially provide a false sense of security for patients. (The AHA does, however, allow for treatment at a blood pressure of 150/90 for adults age 80 and older.)
That being said, if the leading medical organizations don’t agree on when older adults should start seeking treatment for hypertension, it stands to reason that everybody else will be left a little confused on the issue. Only your doctor can look over your entire medical picture (comorbidities, current medications, cardiovascular risk factors, etc.) and make an informed decision about when to prescribe medication for hypertension.
In the meantime, we can all take simple measures to keep our blood pressure low.
The ACP reports that lifestyle changes should often be the first line of treatment, due to fewer side effects and lower financial costs. Their recommendations include the following:
- Lowering sodium
- Following the DASH (Dietary Approaches to Stop Hypertension) diet, which includes plenty of fruits and vegetables, low-fat or non-fat dairy products, whole grains, lean meats, fish, poultry, nuts and beans
- Losing weight
- Exercising
- Lowering alcohol consumption
- Quitting smoking
Tirandaz says that while treating older adults with hypertension can be challenging, it has rewards that can be potentially life-saving.
“Mostly we see the hardening of the arteries that occurs with age,” he says. “Less hardening of the arteries occurs when a person has a better diet, including one that is more plant-based, and when they get more exercise and have lower cholesterol.
“In older people, about 70 percent of all heart failure cases are caused by high blood pressure, which often doesn’t cause signs of illness that you can see or feel. It is a major health problem and is becoming very common in older adults, unfortunately.”
If you are over 60 and know your blood pressure is creeping up, or you aren’t sure what your current blood pressure is, it’s time to see your primary care physician and come up with a plan for keeping hypertension at bay.
Need a primary care physician or heart and vascular specialist? Find a doctor today that suits your needs.

