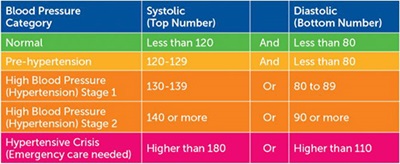
 The American Heart Association considers blood pressure numbers of less than 120/80 mm Hg to be within the normal range. A blood pressure reading above 140/90 mm Hg in pregnancy indicates high blood pressure, or hypertension. Numbers that suddenly rise beyond 180/120 signal that the body is experiencing a hypertensive crisis. Organ function becomes a major concern, along with risk of a heart attack or stroke.
The American Heart Association considers blood pressure numbers of less than 120/80 mm Hg to be within the normal range. A blood pressure reading above 140/90 mm Hg in pregnancy indicates high blood pressure, or hypertension. Numbers that suddenly rise beyond 180/120 signal that the body is experiencing a hypertensive crisis. Organ function becomes a major concern, along with risk of a heart attack or stroke.
Mom-to-be Katie Segall was getting used to having her blood pressure checked at each prenatal appointment. Her numbers always looked good and everything was going fine with her first pregnancy, until it wasn’t.
“At my 28-week ultrasound, the technician looked at my very swollen ankles and asked to take my blood pressure again,” Katie recalls. “It was 150/90 and I was immediately admitted to the hospital for monitoring.”
What Katie was experiencing is a pregnancy complication known as preeclampsia. Preeclampsia is characterized by persistent high blood pressure that develops during pregnancy or postpartum. Thankfully, Katie’s blood pressure stabilized and she was able to be discharged later in the day from Texas Health Dallas to begin bed rest and home monitoring. However, when her numbers began to rise again, the mom-to-be found herself back at the hospital’s high-risk pregnancy care unit. This time, she spent four days in the hospital before her blood pressure stabilized.
After returning home for only one night, Katie’s blood pressure continued to rise. She was once again advised by her doctor to head to Texas Health Dallas, where her numbers continued to skyrocket to 200/120.
“I remember nurse Annie apologizing because she had to call my doctor about my blood pressure,” Katie says. “I was whisked to Labor and Delivery, still in denial and thinking I would soon be back on the high-risk pregnancy care unit. Instead, the on-call doctor came in to tell me that they had to deliver my baby in order to save my life.”
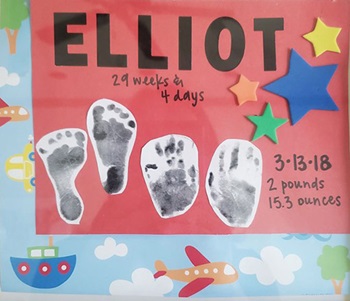 Due to the serious nature of the situation, Katie’s regular doctor, Jane Nokleberg, M.D, an OB/GYN on the medical at Texas Health Dallas, was brought in to perform an emergency C-section. Elliot Segall was delivered at just under 30 weeks. He weighed in at a tiny 2 lbs., 14 oz.
Due to the serious nature of the situation, Katie’s regular doctor, Jane Nokleberg, M.D, an OB/GYN on the medical at Texas Health Dallas, was brought in to perform an emergency C-section. Elliot Segall was delivered at just under 30 weeks. He weighed in at a tiny 2 lbs., 14 oz.
The Bumpy Road to Better Health
Katie needed time to recover from her C-section, and baby Elliot needed time to grow and develop in the hospital’s Level III Neonatal Intensive Care Unit (NICU). Katie admits that those first few days in the hospital were scary. “I was still not doing well, and I was terrified that my son would grow up without me. I forced myself to do laps around the floor to move the fluid out of my body and meditate to bring down my blood pressure, so that I could make trips to the NICU to see my son.”
When Katie was well enough to go home, she did so on blood pressure medication and without little Elliot. One day while visiting Elliott in the NICU, Katie began to not feel well. Upon taking her blood pressure, Katie learned it was 170/100 and she was promptly admitted to the hospital for a fourth time, for another five days.
“We were so lucky to be at Texas Health Dallas,” Katie says. “I stayed in the NICU parent room so I could be close to Elliot. We were lucky that he was strong; he was a grower and feeder.”
“I got to know all the nurses and therapists on the medical staff who took such amazing care of my son and me. Chantal, who was there the day after delivery to help me when I was on magnesium. She also supported me as I learned how to pump. And Katrina, the occupational therapist, who helped Elliot learn to eat. I still have the signs the nurses made for our son. I have one of them framed in his room. It made me feel like he was real and celebrated. One day I had a total break down and our nurse Ashley picked me up and got me back on my feet. There were so many staff members who were special, and at the time, I could only mumble an insufficient thank you,” she adds.
Elliot graduated from the NICU and was moved into the hospital’s Special Care Nursery. In all, he would spend 55 days at Texas Health Dallas. Katie spent nearly every night there so she could maintain a good schedule of feeding him. She read to Elliot from his baby books and told him all about his family and the things they were going to do together once he was home.
“We are so fortunate that he has no repercussions from being forced to join this world 11 weeks early to save his mommy’s life. I tell him every day that he is my hero.”
When asked about her family’s NICU journey and any advice she might have for other expectant moms, Katie simply offers: “Give yourself grace. You are forced to give up your expectations of your birth experience. It can be hard, but know you are not alone.”
To learn more about maternal care at Texas Health, visit TexasHealth.org/Moms.

