DALLAS, Texas — Traffic was beyond congested as Paul Miner drove home just days before Christmas. He took the nearest exit, and then everything went black. “When I regained consciousness, my foot was jammed on the accelerator, the engine was racing, and my rear tires were burning rubber.”
Miner realized he’d exited the major interstate highway, just in the nick of time.
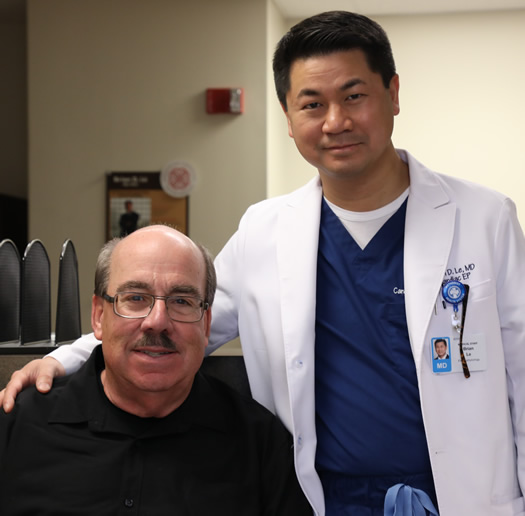
“When it comes to sudden cardiac arrest, you have one chance to make it,” said Brian Le, M.D., a clinical cardiac electrophysiologist with the Texas Health Physicians Group practice* Cardiology and Interventional Vascular Associates (CIVA). “Thanks to a special device, Mr. Miner is alive with no damage to his heart or brain — no disability at all.”
Less than seven days before Miner’s sudden cardiac arrest, Le placed a biventricular pacemaker and implantable cardioverter defibrillator (BivICD) inside his chest. The small, lightweight device detected Miner’s dangerously fast heartbeat (called ventricular fibrillation) sent a shock to his heart, stopped the fast rhythm and restored his heart to a normal heartbeat. The outpatient procedure to implant the device, which lasts about one hour, took place at Texas Health Dallas.
A normal heart rate is between 60 and 100 beats per minute, according to the American Heart Association.
Reviewing data from Miner’s device, Le was able to determine Miner’s heart was racing at well over 300 beats per minute, and that his heart stopped pumping blood for 20 seconds. Le said it takes roughly three seconds of heart-pump cessation for a person to pass out.
“Before I passed out, I felt a little flushed, but I wasn’t in any pain. I didn’t even feel my heart racing,” Miner said. “When I woke up, I had run into a cargo-bed truck, but thankfully, there were no injuries and no major damage to either vehicle. I got myself together and slowly drove home.”
He even waited two weeks before he told his wife he’d almost died.
“With it being the holidays, I didn’t want to cause a big fuss,” Miner said. “But later, Dr. Le told me I was lucky. It could have been a totally different outcome had it not been for the device.”
The battery-operated device is comprised of two major components that help the heart pump normally. The pacemaker doesn’t allow the heart to beat too slowly, while the ICD portion keeps the heart from beating too fast.
Close to 90 percent of Americans who suffer from sudden cardiac arrest outside of the hospital don’t survive, according to the American Heart Association.
“Mr. Miner suffers from cardiomyopathy, which is a disease of the heart muscle that makes it harder for his heart to pump blood to the rest of his body,” said Le. “When it comes to sudden cardiac arrest, medicine doesn’t really address the issue — that’s more so the job of the biventricular ICD.”
When a person suffers from cardiomyopathy, the heart muscle is weak, and the ejection fraction determines how strong the heart muscle is. A normal heart has an ejection fraction between 50 and 70 percent, said Le.
“When it comes to my ejection fraction, my heart function is at 30 percent, which is lower than normal,” Miner said. “But I feel good and I’m improving.”
Miner’s older brother suffers from cardiomyopathy as well. But unlike Miner, he has yet to have the same procedure done.
Miner admits he apprehensively delayed his procedure for three months despite his doctor’s recommendation until his wife’s concern prompted him to take action.
“Most men, I think, also have a tendency to brush away the pain,” Miner said. “You can’t put your health on the back burner though. I keep telling my brother to listen to his doctor, because it saved my life.”
That hesitancy to seek treatment is fairly common, Le said. “He has a lot of life ahead of him. The device helps him feel better while he’s living life and is a guardian angel in his chest.”
*Physicians employed by Texas Health Physician Group practice independently and are not employees or agents of Texas Health Resources hospitals.
Related News
About Texas Health Resources
Texas Health Resources is a faith-based, nonprofit health system that cares for more patients in North Texas than any other provider. With a service area that consists of 16 counties and more than 8 million people, the system is committed to providing quality, coordinated care through its Texas Health Physicians Group and 29 hospital locations under the banners of Texas Health Presbyterian, Texas Health Arlington Memorial, Texas Health Harris Methodist and Texas Health Huguley. Texas Health access points and services, ranging from acute-care hospitals and trauma centers to outpatient facilities and home health and preventive services, provide the full continuum of care for all stages of life. The system has more than 4,400 licensed hospital beds, 6,400 physicians with active staff privileges and nearly 29,000 employees. For more information about Texas Health, call 1-877-THR-WELL, or visit www.TexasHealth.org.
