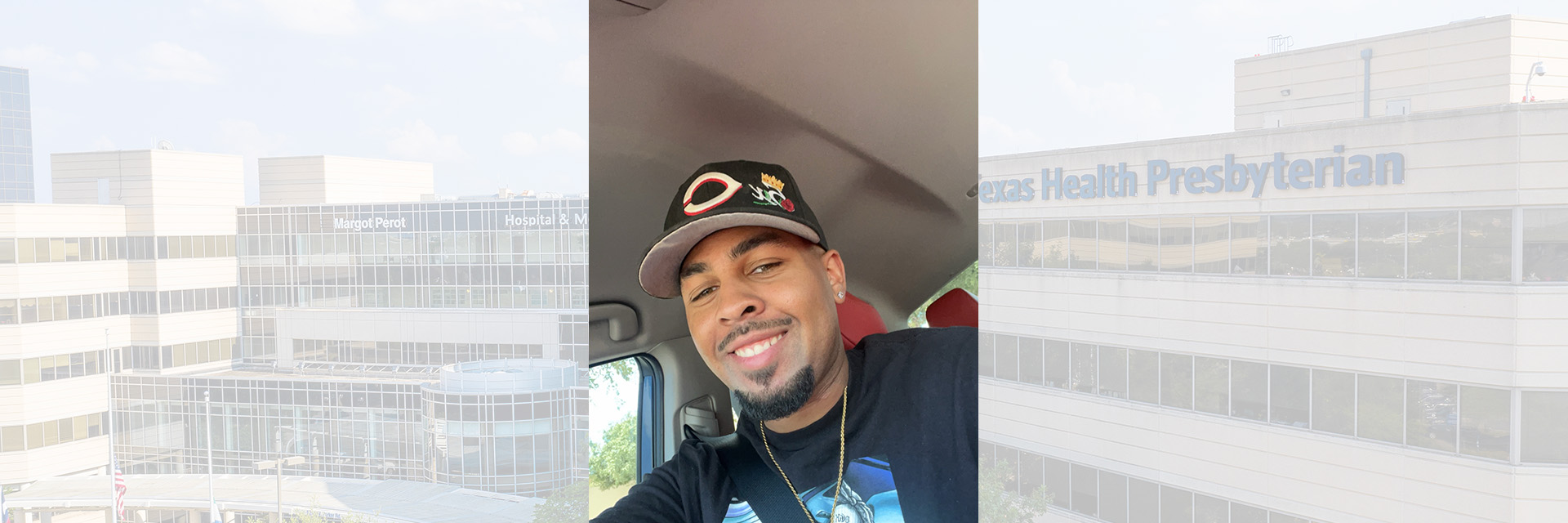
Cameron Love was getting his career off the ground, enjoying time with friends, and living his life as usual. Then he suffered a stroke at the age of 24.
While relatively rare in young people, strokes are becoming more common among adults in the prime of their life. About 10 percent of stroke patients are under the age of 50. The good news is that young stroke survivors with a long life expectancy in front of them can recover to their full potential. Love’s goal is to do just that.
Life Interrupted to Life Regained
The day started like most. Love was up at 6:30 a.m. and preparing to go to work. But on this particular morning in April, the North Texan was plagued by a severe headache. He wasn’t a stranger to headaches, but this one produced “pain like no other.” Love muddled through the discomfort and went about getting ready. That all changed when he began putting on his socks.
“It was weird; the left side of my body went numb and both my legs,” Love says. “My dad was the only other person in the house. I couldn’t get to my phone so I had to beat on the dresser for him to hear me and come.”
When his father found him, the 24-year-old was slurring his speech and his face was drooping on one side. These were symptoms that prompted the responding emergency medical team to take him to the hospital best equipped to provide the proper care.
Advanced Stroke Care in Plano
When Love arrived at Texas Health Presbyterian Hospital Plano, he was taken from the ambulance straight to imaging to be evaluated for possible stroke and to rule out any hemorrhaging in his brain. He was met there by Ryan Cheung, D.O., a neurologist on the hospital’s medical staff. A CT scan revealed that a large vessel occlusion, or clot, had blocked an artery leading to the right side of Love’s brain. As a result, he had suffered an ischemic stroke.
An ischemic stroke occurs when blood flow to the brain is suddenly cut off or interrupted. As a designated Comprehensive Stroke Center, Texas Health Plano offers the highest level of stroke care made possible by physicians on the medical staff who are specially trained in neurointerventions. For Love and other patients with large clots, this means having access to groundbreaking expertise, procedures, and technologies that promote better outcomes.
“People having ischemic stroke can receive clot-busting medication, providing they get it within four and a half hours of the onset of symptoms.,” Cheung explains. “Because he arrived by EMS at 8:25 a.m. and was last seen well when he went to bed the night before, Mr. Love was outside of the usual window to deliver the clot-dissolving medications due to an increased risk of a hemorrhage.”
Instead, Cheung called in Thomas Madaelil, M.D., an interventional neuroradiologist on the hospital’s medical staff, to perform a mechanical thrombectomy with complete reperfusion.
Completion of a mechanical thrombectomy requires a trained team of interventional neuroradiologists, a suite that combines specialized imaging technology with an operating room, and several instruments to navigate the affected blood vessel and ultimately remove the clot.
“Texas Health Plano is fortunate to offer two such surgical suites for patients who need advanced endovascular procedures; this benefits our stroke patients who need that emergent attention,” Madaelil says. “Remarkably, we had just ‘cut the ribbon’ on the second suite 24 hours before Love’s arrival.”
“The suite is equipped with technology that uses two X-ray sources to create detailed, three-dimensional images of blood vessels in the brain, offering clearer images of vascular anatomy and a lesser dose of radiation. It’s also closer to the ER, optimizing our clot retrieval times,” he adds.
Mechanical thrombectomy has changed the landscape of acute ischemic stroke treatment, offering improved outcomes for patients with significant blood clots. Success of the procedure depends on factors such as time elapsed since stroke onset, clot location, and the patient’s overall health.
Although Love has a history of high blood pressure, he was a candidate in part because of his anatomy, and his age. Early imaging had also confirmed that he had not suffered a large stroke so there was viable brain tissue and a likelihood that blood flow could be restored, according to Cheung.
“The goal in mechanical thrombectomy is to implement it as fast as possible. Mr. Love’s case was our fastest door-to-reperfusion time this year so far, with a time of 63 minutes. Successful reperfusion is an important determinant of neurological recovery and is essential to achieving favorable clinical outcomes. A positive outcome was achieved here because everyone was ready at the hospital, the new suite is in the right place, and there was good communication among our multidisciplinary team,” Cheung notes.
The Journey Forward
Love spent only two days in the hospital after his life-saving treatment. He does face occupational and physical therapy for the foreseeable future but says he is making good strides and is looking forward to returning to work.
“I am thankful to Dr. Madaelil and the team for acting immediately. My speech is coming back, the feeling in my left hand is coming back, and I am now able to climb the stairs in my house,” he says.
Learn more about stroke including warning signs and symptoms.
In less than 5-minutes, determine if you could be at risk for stroke with our free stroke risk assessment.