-
Mammography Guidelines
- Women at average risk for breast cancer should start annual mammograms at age 40 and continue through age 74.
- Women who have an increased risk for breast cancer due to family history, a known BRCA1 or BRCA2 gene mutation or other risk factors should discuss screening options with their physician. If you have risk factors, together with your physician you can decide what’s best for you.
-
Risk Factors
Common factors that can increase the chances of developing breast cancer include:
- Age and Gender — Risk of developing breast cancer increases as you get older. The majority of advanced breast cancer cases are found in women over age 50.
- Family History of Breast Cancer — If you have a close relative who has had breast, uterine, ovarian or colon cancer.
- Menstrual Cycle — Women who get their periods early (before age 12) or went through menopause late (after age 55).
- Childbirth — Women who have never had children or who had them only after age 30.
- Obesity — Obesity has been linked to breast cancer, although this link is controversial. The theory is that obese women produce more estrogen, which can fuel the development of breast cancer.
- Radiation — If you received radiation therapy as a child or young adult to treat cancer of the chest area.
- Genes — Certain genes, such as the BRCA1 and BRCA2.
- Alcohol Use — Drinking more than one to two glasses of alcohol a day.
- Diethylstilbestrol (DES) — Women who took DES to prevent miscarriage may have an increased risk of breast cancer after age 40. This drug was given to the women from 1940 to 1960.
- Hormone Replacement Therapy (HRT) — You have a higher risk for breast cancer if you have received HRT for several years or more.
-
Breast Changes
Many breast changes occur in your breast or nipple. You may notice:
- A lump or firmness in your breast or under your arm
- The size or shape of your breast has changed
- Your nipple pointing or facing inward (inverted)
- Your nipple feeling tender
- The skin on your breast, areola or nipple is scaly, red or swollen
- Nipple discharge, or an abnormal fluid coming from the nipple
If you notice any changes in your breast or find a lump, make an appointment with your healthcare provider but don’t panic. Finding a lump can be concerning, but it’s important to remember that most lumps are not cancerous.
-
Breast Surgery
Breast surgeons on the medical staff employ many techniques to surgically treat breast cancer. Talk with your surgeon on the best possible solution for you.
Lumpectomy
A lumpectomy (also known as breast-conserving surgery) removes only the tumor and a small rim of healthy tissue around it. It leaves most of the breast skin and tissue intact.
Mastectomy
A mastectomy is usually recommended if the tumor size is large compared to breast size, if there is more than one area of cancer in the breast, or if the patient cannot undergo radiation therapy.
-
Breast Reconstruction
Breast reconstruction is achieved through several plastic surgery techniques that attempt to restore a breast to near-normal shape, appearance and size following a mastectomy. It can be a physically and an emotionally rewarding procedure for a woman who has lost a breast due to cancer or other condition. For many women, the creation of a new breast can dramatically improve self-image, self-confidence and quality of life.
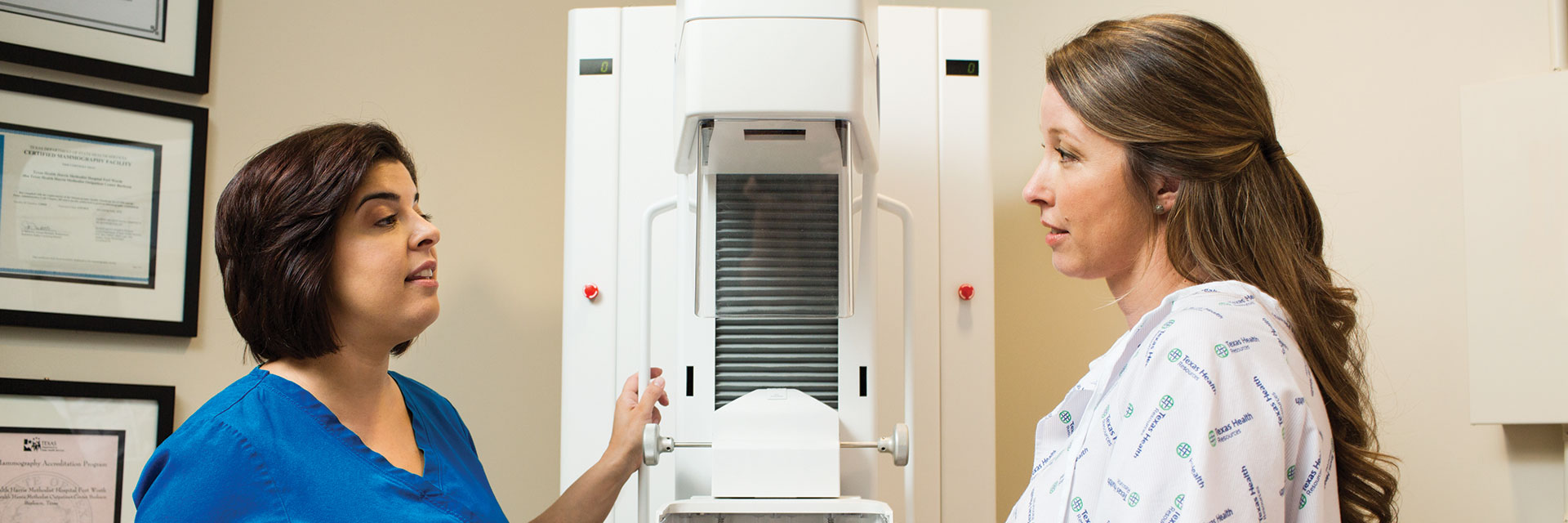
Mammograms can find signs of breast cancer early — often before you can feel a lump during a breast exam. That’s why regular screenings are one of the most important steps you can take to protect your health.
-
Why Choose Texas Health for Your Mammogram?
Breast Care Designed with You in Mind
At Texas Health, we understand that breast health is personal — and so is your experience. That’s why many of our breast centers offer a calming, spa-like environment to help you feel more at ease before your mammogram. From soothing music and private changing areas to refreshment stations and valet parking at select locations, we’ve created spaces that prioritize your comfort.
Advanced Imaging with a Personal Touch
Physicians on the medical staff will recommend the imaging approach that’s most appropriate for your needs. Many centers offer curved paddles and comfort pads to help make your mammogram more comfortable, while still providing the high-quality images needed for diagnosis.
Timely Results You Can Trust
We know waiting can be stressful. That’s why patients are typically contacted as soon as possible with their mammogram results — so you can take the next steps with clarity and confidence.
Convenient Locations Across North Texas
With 18 breast imaging centers throughout the Dallas-Fort Worth area, Texas Health makes it easier to stay proactive about your breast health. Whether it’s your first screening or a follow-up appointment, we’re here to support you — close to home and on your schedule.
-
What Should I Do Before My Appointment?
To help make your visit smooth and comfortable, here are a few things to keep in mind:
- Bring your previous mammogram images if you're a new patient or have them sent ahead of time.
- Wear a two-piece outfit — it makes changing for your exam easier.
- Skip deodorant, powders, body oils, or perfume on the day of your appointment, as they can affect your results.
- Please don’t leave children under 13 unattended in the waiting area.
Cell phones aren’t allowed in exam rooms to help maintain a calm and focused environment.
-
What is a 3D Mammogram?
3D screening mammograms are the preferred type of exam at Texas Health Breast Centers. With a 3D mammogram, the machine takes images of the breast from multiple angles. A computer then creates a 3D image of the breast that the radiologist can examine like pages in a book. Additional benefits include:
- Improves radiologists' ability to screen for and detect potential breast cancers.
- Helps radiologists pinpoint size, shape and location of abnormalities.
- Aids in distinguishing harmless abnormalities from real tumors, leading to fewer callbacks and less anxiety for women.
3D mammograms can also find microcalcifications (tiny deposits of calcium) that sometimes indicate the presence of breast cancer.
-
Will the 3D Mammogram feel Different?
If you have had a mammogram before, you will likely not notice a difference with the exam. During the exam each of your breasts will be compressed between two plates for a few seconds. The breasts will gradually be pressed, and you will be asked to adjust you position several times to take different images. Each breast will be compressed a minimum of two times.
Does My Insurance Cover 3D?
Yes, most insurance plans cover 3D mammography, thanks to Texas House Bill 1036. There are some exceptions, so please verify with your insurance company before the appointment.
If You Are Called Back for Additional Testing
It is fairly routine to receive a request to come back for additional mammogram images or an ultrasound. These additional images may be necessary in order for the radiologist to complete the interpretation of your exam.
-
What is the Difference between a 2D and 3D Mammogram?
A 2D mammogram only takes images of the front and side of the breast, which often overlaps the tissues and can hide certain indicators of cancer. During the 3D portion of the mammogram, images are taken from multiple angles to create a more comprehensive picture of the breast for the radiologists to examine like the pages of a book.
-
Will the Mammogram Hurt?
To get the best images, your breast will be gently positioned between two paddles and gradually compressed. This helps create a clear view for the radiologist. You may feel some pressure or discomfort, but it shouldn’t be painful. If you do feel pain, let your technologist know — they’re there to help make the experience as comfortable as possible.
Curved Comfort Paddles
Many Texas Health Breast Centers offer curved paddles that better match the natural shape of the breast. This helps apply even compression and may reduce discomfort during positioning.Comfort Pads
Some centers also provide cushion pads placed on the machine to create a warmer, softer experience during your exam. -
When Will I Get My Results?
The timing can vary but generally:
- After a screening mammogram, the results will be available in the MyChart app, and they will be mailed to you.
- After a diagnostic mammogram, you will receive your results before you leave your appointment.
- After a biopsy, your ordering provider will receive results within two days after your procedure.




.jpg?h=3969&iar=0&w=6147&hash=8EE849B89D744ACC4C16C23DFE198B19)